Introduction
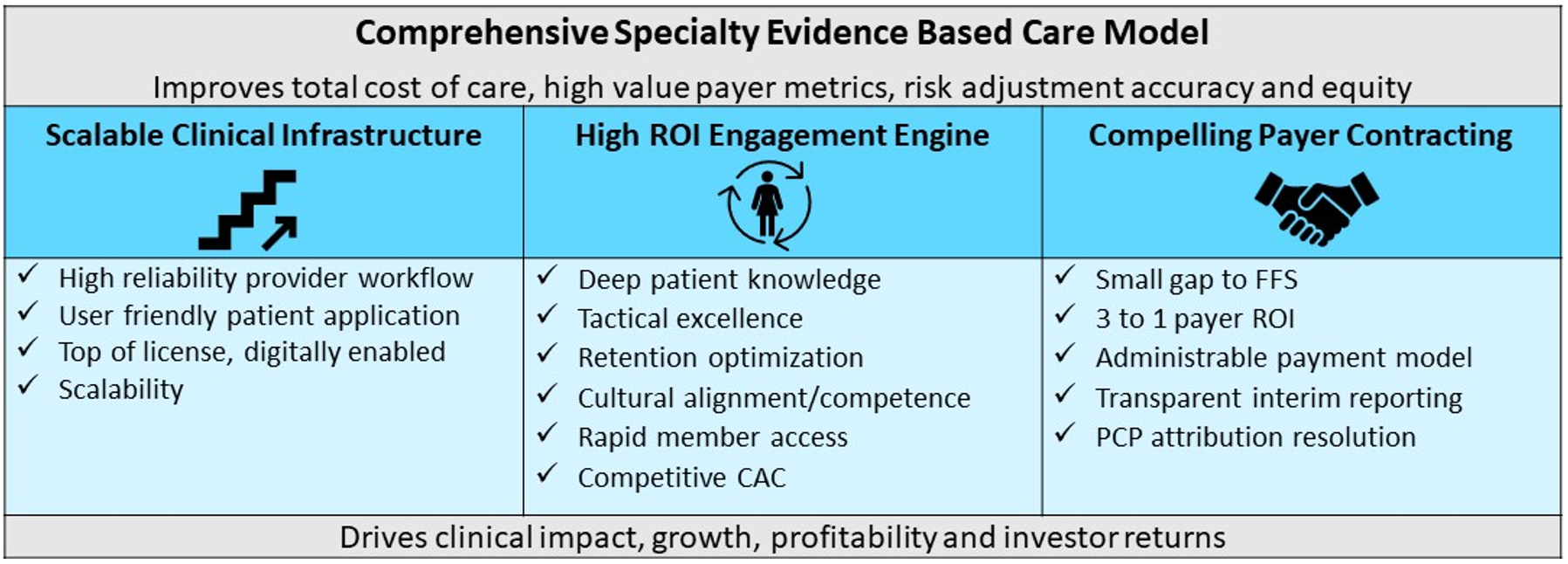
2023 was a difficult year for specialty value based care start-ups. Revenue fell below expectations, engagement lagged and many start-ups struggled. Health system work in this arena was modest despite a critical mass of systems continuing a value based strategy. Yet value based specialty care is essential to address the bulk of total cost of care and quality opportunity that primary care can only indirectly address. Recognizing the need, the Center for Medicare and Medicaid Innovation (CMMI) has established multiple specialty-focused models, including for cancer, kidney disease and bundles for primarily surgical care. Recently added were new models for dementia and severe behavioral health/substance use disorder conditions. Specialty oriented venture-backed companies continue to emerge, offering their products to health plans, employers and directly to consumers. Yet the gap between the promise of these models and broad adoption by patients, payers and employers is still wide. To be successful in this complex environment, high performing models will need to deliver a scalable, seamless clinical infrastructure; a high ROI engagement engine and a compelling payer value proposition.
Checklist for Success
The Care Model
Specialty value based care offerings to attract health plan, employer and CMMI attention must address a clinically coherent, significant source of health care spend. These offerings have the promise to outperform inconsistent and fragmented fee-for-service models in delivering clinical outcomes. The most successful models address frequently overlapping conditions (e.g., a substance use disorder model needs to address the high proportion of members with a serious mental illness). Conditions ripe for these models are often characterized by the ability to substitute medication and lifestyle adherence with real time symptom monitoring/response for costly inpatient and ED care. Diabetes, heart failure and kidney disease are the prototypical examples. Typically, sustaining engagement and addressing SDOH and co-occurring BH conditions are essential elements of the care model. The best models are in‑person/digital hybrids with the ability to adjust for the patient’s preference. Models with deep geographic density combine patient convenience with strong market relationships to drive growth and profitability.
In renal care, companies like Strive and Somatus have leveraged the CMMI Kidney Care Choices model to expand home dialysis technology in a value based framework, alongside more traditional industry players such as DaVita. In a multi-disease context, Evolent has migrated to offering breadth in specialty value based care including oncology, cardiovascular and end-of-life-care. Focusing on employers, digital innovators like Maven in women’s health, Virta in diabetes and Hinge Health in musculoskeletal care have made important inroads.
Early results tend to show cost of care savings in reduced ED visits/inpatient stays, and for some conditions, specialty drug costs (Johnson et al, 2021, BPCI Evaluation, 2021). Other key benefits include more accurate risk adjustment for MA members and targeted quality improvements incented by either the MA Star or state-based Medicaid payer premium methodologies. With strong cultural competence, these models may also substantially reduce disparities.
Within this environment, a checklist can frame success requirements for a specialty value based offering:
- Scalable Clinical Infrastructure
- High ROI Engagement Engine
- Compelling Payer Contracting
Scalable Clinical Infrastructure
Specialty value based care covers many different conditions with a variety of models. There are a number of common infrastructure capabilities that characterize high-performing models.
- Evidence-based, high reliability provider workflow - including specialized documentation, evidence‑based order sets and high productivity scheduling templates.
- User friendly patient application - that combines intelligent remote patient monitoring, a telehealth platform, timely nudges, seamless scheduling and provider communications.
- Top of license care team - structured to optimize existing insurance reimbursable codes (especially early on) and minimize cost.
- Digitally enabled care model - Early results from digital have focused on the orchestration of care rather than pure delivery (e.g., rapid post ED visit follow leveraging HIEs) or stratified clinical decision support to drive tailored care plans, but over time digital care will come to have an increasing impact. Communication with referring partner EMRs is essential.
- Scalability - within and across states. Network models are fastest to scale but require advanced leadership, provider payment models and technology to scale reliably. Staff models bring reliability but significant operating/capital costs. Outsized returns must accompany staff models. The choice of staff versus network model will be influenced by disease prevalence and population density. In geographies where sufficient patient volumes exist to support staff models, the advantages of integration can be realized. In areas of lower population density, where larger geographies must be spanned to reach necessary patient volumes, the network model may be the only real option.
Over time, as real-world evidence tools continue to mature and guide personalized care recommendations, high performing value based care models will bring even greater reliability to delivering the right care to the individual patient.
High ROI Engagement Engine
Effective member engagement is critical and an easy-to-monitor early indicator of program success. That said, it has been very difficult to drive high engagement rates. The common tactics have significant complexity but, once established, can provide a basis of sustainable, competitive advantage. Key approaches include 1. creating access close to patient populations—“feet on the street” in key clinical or community sites, 2. identifying and targeting at risk patients, including digital/telephonic outreach from risk stratified payor lists and/or 3. facilitating patient intake via partnerships with patient navigation engines, at-risk primary care groups or at-risk health systems. New approaches involve participation in widely adopted consumer marketplaces as well as direct-to-consumer models. Success in any of these channels is characterized by:
- Deep patient/customer knowledge - including impactful messaging themes, best access moments and access preferences (channel, time of day, day or week). Machine learning/AI capabilities are already generating actionable insights in this domain establishing an omnichannel learning infrastructure. This customer knowledge needs to be embedded in automated workflows and continuously updated with growing experience.
- Tactical excellence - in each mode of outreach—in person, telephonic and/or digital. Each of these modes has a strong operations logic that requires synchronizing staffing, supporting digital/telephony systems and an underlying CRM that enables outreach to be personalized in each moment. Continuous learning (including leveraging ML/AI) can drive ever high engagement rates. Particularly effective in all modes is timing the outreach to follow an acute ED or inpatient event and continuously refreshing the outreach list for eligibility and clinical condition updates.
- Retention optimization - Continuous learning about the causes of disengagement is required to drive optimization of the model to attack this critical value driver. Minimizing out-of-pocket costs, fostering deep personal relationships with clinical team members and ongoing care convenience (scheduling, prescriptions, provider messaging) are table stakes.
- Cultural alignment/competence - in messaging and staff. All too often, patients don’t engage in needed care over a lack of trust in the outreach. Culturally aligned messaging and staff is a primary trust driver. Selectively, digital content for non-primary English speakers can also drive connection.
- Rapid member access - structured to meet the combination of member availability, clinician availability and clinical need. Like all health care services, an effective offering must address the common mismatch between typical provider availability (daytime, weekdays) and patient availability (evenings, weekends). The match must be structured by provider type for clinical impact within targeted timeframes. Complex disease management places a premium on off hours availability of providers. Unlike routine or elective services, patients with advanced chronic conditions are at risk for decompensation at all hours and every day. Only nuanced provider capacity management supported by the right team incentives, flexible provider scheduling and user-friendly technology can deliver the clinical capability in a way that retains hard to recruit staff.
- Competitive Customer Acquisition Cost (CAC) - At the end of the day, the customer acquisition cost must be affordable within the context of the payment revenue stream.
Compelling Payer Contracting
Specialty based value based care models, typically involving many non-billable services, must be able to execute payer/employer agreements that deliver a return in an administrable contract. In contrast to primary care, the industry lacks standardized models. Payer implementation of a specialty value based care model is challenging given the fee for service administrative/claims payment chassis. Complicating matters, actuarial pricing models are often dependent on billable fee for service equivalency constructs that don’t capture the specialty VBC’s models costs. This gap between the aggregate pricing for FFS billable codes and the resources required for the specialty value based model makes it hard for payer network staff to justify the value based contract to their medical economics staff.
Payer return varies by line of business so the value based specialty care model must deliver operationally against tailored metrics. Solutions that don’t meet these LOB specific drivers will have a hard time gaining traction in the market.
Often the contracting journey that starts with fee-for-service agreements supplemented by payer‑premium generating quality incentives and ideally migrates to greater risk for total cost of care and quality metrics in either a bundled or capitation framework. Critical for cash flow preservation during that first period is minimizing the gap between the historically-based FFS payments and the cost to deliver care. Venture funders prefer models that can break even early in an FFS + quality incentives framework. Leveraging the expanded code sets for care management and SDOH services along with preferred fee for service rates can help. With early results, payer get comfortable increasing the value based elements.
Complicating matters is that innovative payers driving value based care have often started with primary care attributed risk, contractually allocating many lives with their total cost of care budgets to PCP groups. Payers don’t want to “pay twice” for savings on members for these lives. All these factors combine to create a high contracting bar for value based specialty care providers. Successful models will offer:
- Small gap to FFS and provable 3 to 1 payer ROI - To justify an alternative payment model for payers, the successful specialty VBC model must minimize the gap between FFS rates and the cost to deliver services. Shrinking this gap is valuable because it reduces the risk the payer is taking on a higher cost model relative to the traditional FFS alternative. A small gap to FFS lessens the reimbursement burden on complex-to-administer value based payments. That said, getting these agreements over the line also requires a deep understanding of member cost trajectory improvement (relative to regression to the mean) for a payer to justify spending more than the FFS equivalency actuarial model would project. A good rule of thumb is a 3-to-1 payer ROI combing total cost of savings and quality/risk adjustment accuracy-based premium returns.
- Administrable payment model - The market is moving towards a case rate model with risk for quality metrics. This approach is easier to execute for payers who have migrated to case rates more broadly. There are still total cost of care models that combine fee for service (or occasionally capitation) with a back-end reconciliation to share savings. Proof of savings is complex. The gold standard of comparison to a propensity matched cohort is difficult to administer. That said, proving and sharing cost of savings is compelling to all stakeholders. Payers and specialty value based providers are continuing to innovate in this space. Provider side actuarial expertise, either internal or external, is essential.
- Transparent interim reporting - Payer reporting systems, typically dependent on lagged claims reporting, are slow to pick up the benefits of specialty value based care. Strong provider reporting on the volume of unbillable services, rates of member engagement, intermediate outcome measures, clinically documented quality improvement and risk adjustment accuracy outcomes create an environment of trust. This trust is critical as both parties await the lagged claims reporting that demonstrates ultimate total cost of care and quality benefit.
- Primary care attribution conflict resolution - To maximize the number of lives eligible for the model, the specialty VBC provider must address primary care attribution conflicts. A strong position is the reattribution of engaged specialty care patient members where there is no evidence of primary care engagement. Nationally, about a third of members (higher for Medicaid members) don’t identify as having a regular source of primary care even as they are “attributed” to primary care contracting networks. Another option is to negotiate gain share directly with an at-risk primary care provider or health system network on common patients. This approach typically only works with sophisticated at-risk partners with 100% upside/downside risk. Alternatively, some payers may be willing to allocate specialty VBC clinical cost to the primary care provider risk pool (often specifically authorized in the payer value contract with the primary care risk owner), but this tactic is not without friction between the payer and the primary care contractor. Some specialty value based care providers have even considered acquiring their own primary care capability to facilitate attribution. The industry would benefit from stronger payer capabilities on this front enabling both primary care and specialty value based care.
Finally, the models need to generate enough revenue to attract and retain high quality specialists in comparison to their FFS alternatives. Often, these networks start with tapping specialist “excess” capacity, attracting physicians who are supplementing their FFS practice. The strongest performance, however, is earned by practitioners who are wholly steeped in this model. The specialty-based models will need to contract and compensate in a way that can support increasing specialist sustained commitment and mindshare.
A Health System Opportunity As Well?
While traditional views of value based care have often focused on insurers or employers as the “buyers”, health systems may also be able to create economic value by managing their own chronically ill patients more effectively, without the need for risk sharing with payers. For any large hospital or health system, roughly 10% to 15% of their individual patients are connected with enormous financial losses as revenue falls short of covering costs. Much of the care being delivered at a loss involves avoidable utilization that an effective chronic episode management program could significantly reduce. The same value proposition that applies for external contracting—namely, the ability to reduce avoidable costs associated with chronically ill patients—applies to a health system’s own existing patient population, particularly when covered by government payers or uninsured altogether. A disease management offering can be developed for a provider’s own patients, who can create the foundation for scale. Once successful intramurally, the program is more likely to thrive externally in relationship with third-party payers. Taking on this challenge must be supported by sophisticated financial modeling and, for some, supports any primary care risk offerings.
Looking Forward
The complex checklist capabilities are enabled by both human process and technology. Fortunately, as the technology tools have advanced rapidly in the last five years, even the MVP versions of these capabilities can deliver value. It is critical to have a roadmap that is focused on early success drivers that lays a longer-term foundation for differentiated performance.
In 2024, specialty-based providers that can deliver savings and quality outcomes to payers will see growth as they overcome these clinical, engagement and contracting challenges. There are multiple market signals. MA continues to grow. CMMI continues to make progress towards its goal of driving 100% of Medicare FFS members into value based care. State Medicaid procurement rules increasingly stress the proportion of care governed by value based arrangements. Employers continue to hunger for more effective value based strategies to combat continued health care inflation and reduce employee burden from high deductible plans.
With the right clinical model, clinical infrastructure, member engagement model and value based care contracting structure, specialty value based care providers can be positioned to deliver outstanding results, scale and consider exit opportunities.
Acknowledgments
The authors would like to acknowledge Manatt’s Tracy Massel and Tom Robertson for their thoughtful contributions to this article.